Cleaning Validation in Medical Devices: Safety and Quality
Why Residue/Cleanliness Validation is Necessary?
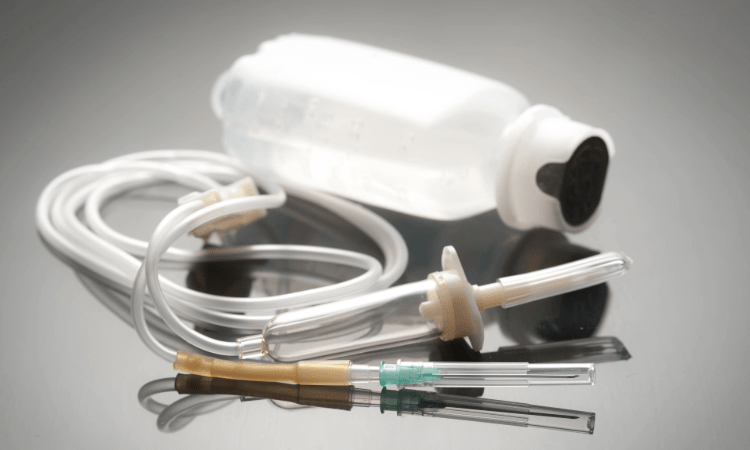
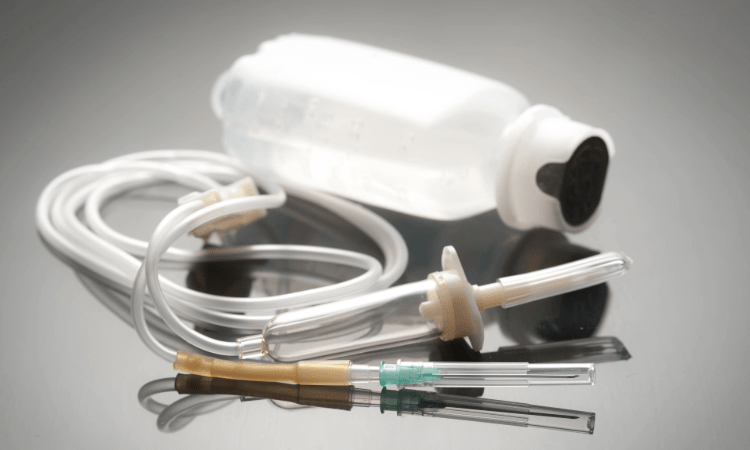
The sterility, cleanliness and reliability of medical products and medical devices are of great importance for patient health and safety. Chemicals, oils and other residual materials used in the manufacturing processes of these devices can remain on the surfaces of the devices, and these residues can pose a risk. Residue/cleanliness validation is a vital process to verify the cleanliness of devices and ensure their safe use.
What is Residue/Cleanliness Validation?
Residue/cleanliness validation is an assessment process that tests whether chemical, biological or physical residues left on the surfaces of medical devices and
medical products are within specified limits. The aim of this process is to prove that the devices are clean and free from contamination, thus preventing any risk to patient health.
Why Residue/Cleanliness Validation is Necessary?
It is quite common for medical products and medical devices to come into contact with chemicals during the manufacturing, assembly or sterilization stages, or to leave residues from lubricants and cleaners used in the manufacturing process. These residues can pose a risk to both patient safety and device effectiveness. The main benefits of validation are:
- Patient Safety: Residues can lead to risk of infection or toxic effects. Cleaning validation ensures the safe use of devices.
- Compliance and Certification: According to standards from regulatory bodies such as ISO 13485 and the FDA, the cleanliness of medical devices must be mandatorily tested. Residue/cleanliness validation ensures compliance with these regulatory requirements.
- Product Reliability: Cleaning validation guarantees the quality of the instrument, increasing its long-term reliability.
Standards in Cleaning Validation
Various worldwide standards guide the medical product and medical device cleaning validation process. These standards set residue limits and ensure the safe use of the device.
- ISO 13485: This standard specifies the requirements for quality management systems in medical device manufacturing. Cleaning and residue control are part of this system.
- ISO 19227: This standard for the cleaning of medical devices specifically covers residue analysis and cleaning of surgical implants and medical devices.
- FDA Guidelines: The U.S. Food and Drug Administration (FDA) provides detailed guidelines on cleaning validation and mandates staying below certain residue levels.
Residue/Cleanliness Validation Process
Residue/cleanliness validation is performed according to specific standards and methodologies. Here are the key stages of the cleaning validation process:
- Cleaning Method Selection: The appropriate cleaning method is determined according to the production process. Different methods such as ultrasonic cleaning, washing with chemical cleaners or using compressed air can be preferred.
- Determination of Residue Limits: The amount of residue that can be left in the product is determined. These limits vary according to the intended use and material of the product.
- Selection of Analysis Methods: Analysis methods to be used for residue detection are selected. Chemical analysis methods such as FTIR, HPLC, GC-MS are generally used. These are preferred according to the type of residue.
- Performing the Tests: Residue analysis is performed on the device. These tests determine the amount of chemicals remaining on the surface of the device and determine whether they are within the specified limits.
- Data Analysis and Reporting: Test results are analyzed and compared to the set residue limits. At the end of this process, the device is certified as safe and clean.
What Tests/Analyses are Performed in Cleaning Validation?
1. Organic Residue Tests
- TOC (Total Organic Carbon) Analysis: Used for the detection of organic residues left on the surface. It is a critical parameter for evaluating the effectiveness of cleaning processes.
- Protein Testing: It is applied to detect protein residues. It is especially preferred for surgical instruments.
- UV Spectroscopy: Used to detect soluble organic residues.
- Oil and Lubricant Analysis: It is checked whether the oils and greases used in the production process are cleaned.
2. Physical and Chemical Residue Tests
- Ionic Residue Tests:
- Chloride and Sulfate Analysis: Determination of ionic contaminants remaining on the surface.
- Conductivity Test: To assess the concentration of ionic residues on the surface.
- pH Test: Checks the neutralization of residues left after cleaning.
- ICP-OES/ICP-MS (Inductively Coupled Plasma): To detect heavy metal residues from the manufacturing processes of medical products.
- AAS (Atomic Absorption Spectroscopy): To measure the presence of metal ions.
- Detergent Residue Analysis: To evaluate whether the detergents used during cleaning remain on the surface.
- GC-MS (Gas Chromatography-Mass Spectrometry): For the detection of organic solvent residues.
- Visual Particle Test: Checks for visible particles on the product surface after cleaning.
- VOC (Volatile Organic Compound) Analysis: To detect gas residues, especially in ethylene oxide sterilized products.
- Water Soluble Residue Tests: Soluble residues remaining after water-based cleaning can be analyzed by ion chromatography or conductivity meter
- Ethylene Oxide (ETO) Sterilization Residue Tests: The soluble residues remaining after sterilization can be analyzed as ETO, ECH, EG with GC-FID device.
3. Biological Residue Tests
- Biological Load (Bioburden) Test: Used to determine the number and type of microorganisms on the surface of medical devices.
- Endotoxin Test (LAL - Limulus Amebocyte Lysate Test): Checks for the presence of bacterial endotoxin in medical products. It is especially necessary on critical devices such as implants.
- Sterility Tests: To assess whether biological residues left after cleaning are eliminated during sterilization.
- Swab Test: Analyzes cleaning effectiveness by sampling the surface of the device.
Why NANOLAB?
Nanolab offers the most reliable and fastest solution for cleaning validation in medical products and medical devices with its experience in the sector and strong infrastructure. It meticulously analyzes residues on the surfaces of products to verify the effectiveness of cleaning processes and determines whether cleaning procedures fully meet safety and quality requirements. Thanks to ISO 17025 accreditation, validation results are internationally recognized and the biological safety and suitability of products is accurately assessed. With its wide range of equipment and expert technical team, it completes cleaning validation processes efficiently and quickly. Thanks to its regulatory expertise, relevant standards and legal requirements are fully met. Nanolab stands out as the address where quality, reliability and speed combine in cleaning validation of medical products and medical devices.
For more information, please contact us.
You can follow us on LinkedIn for the latest news and updates about our services.
Follow our Instagram account to stay up to date with our latest blog posts.